It may not feel like it, but summer will soon be upon us. This means ample opportunity to walk around with your shirt off and impress everyone. But right now that may not be such an appealing idea. One thing that winter always provides is a few extra inches around the waist, and a determination that you’ll be ripped by summer. But how do you go about getting shredded between now and the end of spring? Well this article will help you get there. We are going to look at five ways to get shredded this summer. Tip #1: Take stock of your current situation Before making any plans you really should take a good look at where you are currently at physique and fitness wise . If you are borderline obese and haven’t run 100m since high school then jumping into a 5 times per week crossfit program is probably not going to lead to good results! But even if you are in decent shape, you will still get huge benefits from assessing yo...
What are the kidneys and what do they do?
The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the two kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid. Children produce less urine than adults and the amount produced depends on their age. The kidneys work around the clock; a person does not control what they do. Ureters are the thin tubes of muscle—one on each side of the bladder—that carry urine from each of the kidneys to the bladder. The bladder stores urine until the person finds an appropriate time and place to urinate.Kidneys work at the microscopic level. The kidney is not one large filter. Each kidney is made up of about a million filtering units called nephrons. Each nephron filters a small amount of blood. The nephron includes a filter, called the glomerulus, and a tubule. The nephrons work through a two-step process. The glomerulus lets fluid and waste products pass through it; however, it prevents blood cells and large molecules, mostly proteins, from passing. The filtered fluid then passes through the tubule, which sends needed minerals back to the bloodstream and removes wastes. The final product becomes urine.
The kidneys also control the level of minerals such as sodium, phosphorus, and potassium in the body, and they produce an important hormone to prevent anemia. Anemia is a condition in which the number of red blood cells is less than normal, resulting in less oxygen carried to the body’s cells.

What is kidney failure and how is it treated in children?
Kidney failure—described as end-stage kidney disease or ESRD when treated with a kidney transplant or blood-filtering treatments called dialysis—means the kidneys no longer work well enough to do their job. In most cases, kidney failure in children is treated with a kidney transplant. Though some children receive a kidney transplant before their kidneys fail completely, many children begin with dialysis to stay healthy until they can have a transplant.Dialysis is the process of filtering wastes and extra fluid from the body by means other than the kidneys. Sometimes, a transplanted kidney may stop working, and the child may need to return to dialysis. Transplantation may be delayed if a matching kidney is not available or if the child has an infectious disease or an active kidney disease that has progressed rapidly.
What are the types of dialysis?
Hemodialysis and peritoneal dialysis are the two types of dialysis.Hemodialysis
Hemodialysis uses a special filter called a dialyzer to remove wastes and extra fluid from the blood. The dialyzer is connected to a hemodialysis machine. Blood is pumped through a tube into the dialyzer to filter out the wastes and extra fluid. The filtered blood then flows through another tube back into the body. The hemodialysis machine monitors the process to keep blood moving at a safe pace. Hemodialysis helps control blood pressure and helps the body maintain the proper balance of important minerals, such as potassium, sodium, calcium, and bicarbonate.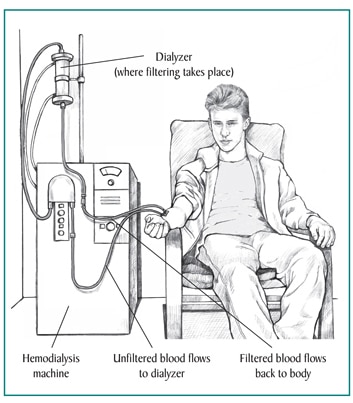
Some dialysis centers teach parents or guardians how to perform their child’s hemodialysis at home. Having treatments at home allows for longer or more frequent dialysis, which comes closer to replacing the steady work healthy kidneys do.
- Daily home hemodialysis is done 5 to 7 days per week for 2 to 3 hours at a time.
- Another option is to perform hemodialysis at home 3 to 6 nights a week while the child sleeps.
- Though home hemodialysis allows more flexibility in scheduling and may have better results, learning how to perform the procedure often takes 3 to 8 weeks.
- infection
- poor blood flow
- blockage from a blood clot
Rapid changes in the body’s fluid and mineral balance during treatment may cause other problems with hemodialysis treatments. Muscle cramps and hypotension—a sudden drop in blood pressure—are two common side effects. Hypotension can make a child feel weak, dizzy, or nauseous. A health care provider can treat these problems with adjustments to the dialysis solution prescription and the speed at which blood flows through the dialyzer.
Most children need a few months to adjust to hemodialysis. A health care provider can often quickly and easily treat side effects, so a parent or guardian should always report side effects to a member of the health care team. A parent or guardian can help a child prevent many side effects by making sure the child maintains a proper diet, limits liquid intake, and takes all medications as directed. See "Eating, Diet, and Nutrition" for more information on how the right food choices can help.
More information is provided in the NIDDK health topic, Treatment Methods for Kidney Failure: Hemodialysis.
Peritoneal Dialysis
Peritoneal dialysis uses the lining of the abdominal cavity—the space in the body that holds organs such as the stomach, intestines, and liver—to filter the blood. The lining is called the peritoneum. A kind of salty water called dialysis solution is emptied from a plastic bag through a catheter—a thin, flexible tube—into the abdominal cavity. While it is inside, the dialysis solution soaks up wastes and extra fluid from the body. After a few hours, the used dialysis solution is drained into another bag, removing the wastes and extra fluid from the body. The abdomen is filled with fluid all day and all night, so the filtering process never stops. The process of draining and refilling, called an exchange, takes about 30 minutes.Before peritoneal dialysis begins, a surgeon places a catheter into the child’s abdomen. The catheter insertion may be done as an outpatient procedure, or the child may need to stay overnight in the hospital. The catheter tends to work better if the insertion site, also known as the exit site, has adequate time to heal—usually 10 to 20 days. The catheter may have one or two cuffs that the abdominal tissue grows around to secure it in place.
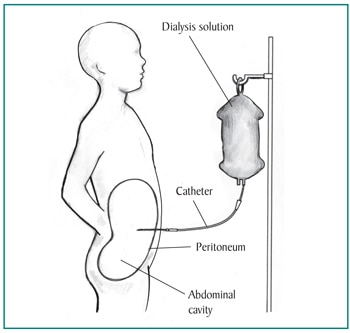
- Continuous ambulatory peritoneal dialysis (CAPD). CAPD requires no machine and can be done in any clean, well-lit place. With CAPD, the blood is always being filtered. The dialysis solution stays in the abdomen for 4 to 6 hours or more between exchanges, called dwell time. Most children change the dialysis solution at least four times a day and sleep with solution in their abdominal cavity at night. With CAPD, it is not necessary to wake up and perform dialysis tasks during the night.
- Continuous cycling peritoneal dialysis (CCPD). CCPD uses a machine called a cycler to fill and empty the abdomen three to five times during the night while a child sleeps. In the morning, the abdomen is filled with dialysis solution for a dwell time that lasts the entire day. Sometimes, an additional exchange can be done in the middle of the afternoon without the cycler to increase the amount of waste removed and to reduce the amount of fluid left behind in the body.
The most common problem with peritoneal dialysis is development of peritonitis, a serious infection of the peritoneum. This infection can occur if the exit site becomes infected or if contamination occurs as the catheter is connected to, or disconnected from, the bags of dialysis solution. Peritonitis is treated with bacteria-fighting medications called antibiotics.
To prevent peritonitis, those performing peritoneal dialysis tasks should wear a surgical mask, follow procedures exactly, and learn to recognize the early signs of peritonitis, including
- fever
- nausea or vomiting
- redness or pain around the catheter insertion site
- unusual color or cloudiness in used dialysis solution
- a catheter cuff that has been pushed out of the body
What is kidney transplantation?
Kidney transplantation is surgery to place a healthy kidney from someone who has just died or a living donor, usually a family member, into a person’s body to take over the job of the failing kidney. Once kidneys fail because of chronic kidney disease (CKD), function cannot be restored, so transplantation is the closest thing to a cure. Children with a transplant will need to take medications every day to prevent their body from rejecting the new kidney and get regular checkups to make sure the new kidney is accepted and functioning properly.To receive a donor kidney, a child first undergoes a thorough medical evaluation at a transplant center.
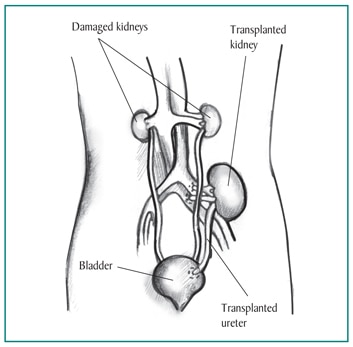
Deceased Donor Kidneys
If the medical evaluation shows that the child does not have a condition that would prevent a successful transplant, the transplant coordinator places the child on a waiting list.Transplant coordinators register those needing a deceased donor organ with the United Network for Organ Sharing (UNOS), which maintains a centralized computer network linking all regional organ procurement organizations (OPOs) and transplant centers. A child can be registered with multiple transplant centers; most centers require a separate medical evaluation.
The length of time a child has to wait for a transplant depends on many things; however, it is determined primarily by how good the match is between the child and the donor. A child’s place on the list depends on the following:
- tissue typing—a blood test that checks six antigens, or proteins, that make each person different. Tissue typing lets the transplant surgeon know how many antigens the donor shares with the recipient.
- blood type.
- length of time on the waiting list.
- age of child waiting.
- blood antibody levels, which show how active the immune system is at the current time, a factor than can increase the risk of rejection. The immune system normally protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances.
Living Donor Kidneys
About half of the kidneys transplanted into children are from living donors, often a parent, family member, or family friend.1 Potential donors need to be tested for matching factors and to make sure that donating a kidney will not endanger their health.A kidney from a living donor often has advantages over a kidney from a deceased donor because
- a kidney from a parent is more likely to be a better tissue match than a kidney from someone who is not related to the child
- living donation allows for greater preparation; for example, the operation can be scheduled in advance
- the kidney does not have to be transported from one site to another, so it may be in better condition
Preemptive Transplantation
Preemptive transplantation is when a child receives a donated kidney before dialysis is needed. Some studies indicate that preemptive transplantation reduces the chances of the body rejecting the new kidney and improves the chances of the new kidney functioning for a long time. Other studies show little or no advantage to preemptive transplants, although some families may feel that avoiding dialysis is itself an advantage.What are the possible complications for children with a kidney transplant?
Children with a kidney transplant are at risk for complications such as organ rejection, infection, and certain types of cancer. They may also need treatment to increase their growth rate.Organ Rejection
The body’s immune system can attack transplanted organs. This reaction is known as rejection. Children with a kidney transplant need to take immunosuppressive medications to prevent the body from making antibodies and rejecting the kidney. Many children have a hard time following the treatment regimen. Health care providers use the term nonadherence to describe the failure or refusal to take prescribed medications or follow a health care provider’s directions. Adherence can be improved with a combination of health education, motivational techniques, and behavioral skill methods. Strategies need to be tailored to each child and the child’s family. The health care provider should- teach the child about the condition and treatment regimen
- talk with the child to learn about the child’s wishes, beliefs, and feelings to find ways to improve motivation
- suggest methods for remembering to take medications, such as a calendar, a pillbox, or text message reminders
Infection
Immunosuppressive medications can leave children vulnerable to infections and can also prevent the body from responding to vaccines. While children should get the standard vaccines as well as vaccines against influenza and pneumonia prior to transplantation, they may need to wait several months after the transplant before they get any additional vaccines. Children who take immunosuppressive medications should not receive vaccines containing live viruses, such as the- oral polio vaccine
- measles, mumps, and rubella (MMR) vaccine
- varicella or chicken pox vaccine
- avoid contact with people who are ill
- wash their hands often
- avoid raw or undercooked meats
- wear gloves when gardening or working outdoors
- avoid caring for pets
- report any signs or symptoms to the health care team right away
Cancer
Over a long period of time, children taking immunosuppressive medications may develop some forms of cancer. Cancer most often develops in the skin or lymph cells, part of the body’s immune system. The incidence of cancer in pediatric transplant recipients is lower than in adults, with the risk being about 17 percent within 25 years of receiving the transplant.2Growth Rate
Depending on their age at the time of the transplant, how well the transplanted kidney is working, and medication dosing, children may have an increase in growth after receiving a transplant, though they are typically shorter than average height. Children younger than 4 years old have the best growth rate after transplantation.2 However, high doses of immunosuppressive medications can slow a child’s growth and development after a transplant. Decreasing immunosuppressive medication dosing and giving the child growth hormone can improve growth rate.What are the complications of kidney failure and how are they treated?
Children with kidney failure may also need treatment for complications such as anemia, bone problems and growth failure, and infection. These complications are caused by the inability of the damaged kidneys to make red blood cells, balance nutrients needed for strong bones and growth, or filter wastes and extra fluid from the blood.Anemia
Damaged kidneys do not make enough of a hormone called erythropoietin (EPO), which stimulates the bone marrow to produce red blood cells. Anemia is common in children with kidney disease and causes them to tire easily and look pale. Anemia may also contribute to heart problems. A synthetic form of EPO injected under the skin one or more times a week can treat anemia caused by damaged kidneys.Bone Problems and Growth Failure
The kidneys help bones stay healthy by balancing phosphorus and calcium levels in the blood. When the kidneys stop working, phosphorus levels in the blood can rise and interfere with bone formation and normal growth. When phosphorus levels become too high, a health care provider may prescribe medications to decrease blood phosphorus levels and increase blood calcium levels.A health care provider may recommend dietary changes and food supplements or growth hormone injections to treat growth failure in children.
Infection
The wastes and toxins that build up in the bloodstream of children with kidney disease can weaken the immune system, making children vulnerable to certain infections and diseases. Vaccinations can help prevent certain infections, which is particularly important for children with a weakened immune system. Children with kidney failure should receive the standard vaccinations recommended for all children, as well as vaccinations to prevent influenza and pneumonia.What are the challenges of kidney failure for children and their families?
The challenges of kidney failure for children include physical effects from the loss of kidney function and emotional effects due to their illness. Physical effects of kidney failure can include- extreme fatigue
- weak bones
- nerve damage
- sleep problems
- growth failure
Emotional effects of kidney failure can include depression and feelings of isolation, which is especially a problem for children, who place great importance on making friends and fitting in. Children with kidney failure may need individualized plans to help them become active, productive, well-adjusted adults.
The challenges for families caring for a child with kidney failure can include understanding treatment options, scheduling and performing dialysis, and learning how to keep the child as healthy as possible. Family members should feel comfortable talking to any member of their child’s health care team about their concerns and questions. Working closely with the health care team can make life easier for children with kidney failure and for their families.
Who is on the health care team for children with kidney failure?
The following skilled professionals may be on a child’s health care team:- pediatrician
- nephrologist
- dialysis nurse
- transplant coordinator
- transplant surgeon
- social worker
- mental health professional
- financial counselor
- dietitian
Pediatrician
A pediatrician is a doctor who treats children. A child’s pediatrician is likely to be the first to recognize a kidney problem—either during a routine physical exam or during a sick visit. Depending on how well the kidneys are working, the pediatrician may decide to monitor the child or refer the child to a specialist. The pediatrician should talk with any specialists who become involved. A consultation with a specialist should occur soon after CKD is diagnosed, even if dialysis and transplantation are still a long way off.Nephrologist
A nephrologist is a doctor who treats kidney diseases and kidney failure. A child should see a pediatric nephrologist if possible because they are specially trained to take care of kidney problems in children. In many parts of the country, pediatric nephrologists are in short supply, so the child may need to travel. If traveling is not possible, some nephrologists who treat adults can also treat children in consultation with a pediatric nephrologist.The nephrologist may prescribe treatments to slow disease progression and will determine when referral to a dialysis clinic or transplant center is appropriate.
Dialysis Nurse
If the child needs dialysis, a nurse with special training will make sure all procedures are followed carefully:- For peritoneal dialysis, the dialysis nurse will train the parents or guardians so they feel comfortable performing exchanges at home.
- For hemodialysis in a clinic, the dialysis nurse will make sure all needles are placed correctly and watch for any problems.
- The dialysis nurse can discuss the advantages and disadvantages of the different types of dialysis and explain how well the treatments are working.
Transplant Coordinator
When preparing for a transplant, children and their families work with a coordinator at a transplant center, who serves as their main contact. The coordinator- schedules any required exams and procedures
- ensures the child’s medical information is complete
- places the child on the UNOS national waiting list
- makes sure every member of the child’s health care team has all of the necessary information and paperwork
Transplant Surgeon
The transplant surgeon performs the kidney transplant and monitors a child’s health before the surgery. Children waiting for a transplant need to stay as healthy as possible. After the surgery, the transplant surgeon will make sure the new kidney is working well.Social Worker
Every dialysis clinic and transplant center has a social worker who can help families locate services such as transportation and family counseling. The social worker can provide information about- finding support groups in the community
- helping a child with a chronic illness rejoin school activities
- reducing the stress of caring for a child with a chronic illness
Mental Health Professional
A mental health professional, such as a psychologist, can help children with CKD find useful ways to deal with the emotional turmoil caused by having a chronic illness. Some child psychologists specialize in helping children with disabilities and medical problems rejoin school activities. They may be able to suggest ideas that reinforce adherence with taking medication and following the health care provider’s instructions.Family members may also find that counseling helps them handle the conflicts and stresses they face. Many couples report increased tension in their marriage when their child has a serious illness such as CKD. Siblings may resent the amount of attention given to their sibling with CKD and feel guilty about having bad thoughts about their sibling.
Financial Counselor
A financial counselor can help families meet the financial obligations that chronic illness creates. Medical bills can strain family finances; in some cases, a parent or guardian may need to stop working to care for a child full time.Dietitian
Proper nutrition is extremely important for children with CKD. Every dialysis clinic has a dietitian to help people understand how the food they eat affects their health. The dietitian- helps develop meal plans to fit a child’s restricted diet
- provides information about possible nutritional deficiencies caused by kidney disease
- recommends special dietary supplements or formulas to improve the child’s nutrition
- provides recipes and recommends cookbooks appropriate for people with kidney disease
Eating, Diet, and Nutrition
For children with CKD, learning about nutrition is vital because their diet can affect how well their kidneys work. Parents or guardians should always consult with their child’s health care team before making any dietary changes. Staying healthy with CKD requires paying close attention to the following elements of a diet:- Protein. Children with CKD should eat enough
protein for growth while limiting high protein intake. Too much protein
can put an extra burden on the kidneys and cause kidney function to
decline faster. Protein needs increase when a child is on dialysis
because the dialysis process removes protein from the child’s blood. The
health care team recommends the amount of protein needed for the child.
Foods with protein include
- eggs
- milk
- cheese
- chicken
- fish
- red meats
- beans
- yogurt
- cottage cheese
- Sodium. The amount of sodium children need
depends on the stage of their kidney disease, their age, and sometimes
other factors. The health care team may recommend limiting or adding
sodium and salt to the diet. Foods high in sodium include
- canned foods
- some frozen foods
- most processed foods
- some snack foods, such as chips and crackers
- Potassium. Potassium levels need to stay in the
normal range for children with CKD, because too little or too much
potassium can cause heart and muscle problems. Children may need to stay
away from some fruits and vegetables or reduce the number of servings
and portion sizes to make sure they do not take in too much potassium.
The health care team recommends the amount of potassium a child needs.
Low-potassium fruits and vegetables include
- apples
- cranberries
- strawberries
- blueberries
- raspberries
- pineapple
- cabbage
- boiled cauliflower
- mustard greens
- uncooked broccoli
High-potassium fruits and vegetables include - oranges
- melons
- apricots
- bananas
- potatoes
- tomatoes
- sweet potatoes
- cooked spinach
- cooked broccoli
- Phosphorus. Children with CKD need to control
the level of phosphorus in their blood because too much phosphorus pulls
calcium from the bones, making them weaker and more likely to break.
Too much phosphorus also can cause itchy skin and red eyes. As CKD
progresses, a child may need to take a phosphate binder with meals to
lower the concentration of phosphorus in the blood. Phosphorus is found
in high-protein foods. Foods with low levels of phosphorus include
- liquid nondairy creamer
- green beans
- popcorn
- unprocessed meats from a butcher
- lemon-lime soda
- root beer
- powdered iced tea and lemonade mixes
- rice and corn cereals
- egg white
- sorbet
- Fluids. Early in CKD, a child’s damaged kidneys may produce either too much or too little urine, which can lead to swelling or dehydration. As CKD progresses, children may need to limit fluid intake. The health care provider will tell the child and parents or guardians the goal for fluid intake.
Points to Remember
- Kidney failure—described as end-stage kidney disease or ESRD when treated with a kidney transplant or blood-filtering treatments called dialysis—means the kidneys no longer work well enough to do their job.
- In most cases, kidney failure in children is treated with a kidney transplant. Though some children receive a kidney transplant before their kidneys fail completely, many children begin with dialysis to stay healthy until they can have a transplant.
- Dialysis is the process of filtering wastes and extra fluid from the body by means other than the kidneys. Hemodialysis and peritoneal dialysis are the two types of dialysis.
- Hemodialysis uses a special filter called a dialyzer to remove wastes and extra fluid from the blood. The dialyzer is connected to a hemodialysis machine. Blood is pumped through a tube into the dialyzer, which uses a dialysis solution to filter out the wastes and extra fluid. The filtered blood then flows through another tube back into the body.
- Peritoneal dialysis uses the lining of the abdominal cavity—the space in the body that holds organs such as the stomach, intestines, and liver—to filter the blood.
- Kidney transplantation is surgery to place a healthy kidney from someone who has just died or a living donor, usually a family member, into a person’s body to take over the job of the failing kidney.
- Children with a kidney transplant are at risk for complications such as organ rejection, infection, and certain types of cancer. They may also need treatment to increase their growth rate.
- Children with kidney failure may also need treatment for complications such as anemia, bone problems and growth failure, and infection. These complications are caused by the inability of the damaged kidneys to make red blood cells, balance nutrients needed for strong bones and growth, or filter wastes and extra fluid from the blood.
- The challenges of kidney failure for children include physical effects from the loss of kidney function and emotional effects due to their illness.
- The challenges for families caring for a child with kidney failure can include understanding treatment options, scheduling and performing dialysis, and learning how to keep the child as healthy as possible.
- The following skilled professionals may be on a child’s health care team:
- pediatrician
- nephrologist
- dialysis nurse
- transplant coordinator
- transplant surgeon
- social worker
- mental health professional
- financial counselor
- dietitian
- Parents or guardians, however, are the most important members of a child’s team.
- For children with chronic kidney disease (CKD), learning about nutrition is vital because their diet can affect how well their kidneys work. Parents or guardians should always consult with their child’s health care team before making any dietary changes.
Comments
Post a Comment